There’s a condition that is not well understood. It creates a lot of common signs and symptoms: headache, dizziness, tinnitus, and a few others. But it hides a lurking danger: weak blood vessels that may bulge in some places and become dangerously narrow in others. It can contribute to stroke and kidney damage. It is usually found only by accident, during testing for other issues. Fortunately, it is fairly rare.
What is it, and what are the cautions for massage therapy for people who have it?
Listen in for more on fibromuscular dysplasia.
Resources: 
Pocket Pathology: abmp.com/abmp-pocket-pathology-app
"Fibromuscular Dysplasia" (no date) NORD (National Organization for Rare Disorders). Available at: https://rarediseases.org/rare-diseases/fibromuscular-dysplasia/ (Accessed: 25 January 2022).
"Fibromuscular Dysplasia" (FMD) (no date). Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/fibromuscular-dysplasia-fmd (Accessed: 25 January 2022).
"Fibromuscular Dysplasia" (FMD): Types, Symptoms & Treatment (no date) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/17001-fibromuscular-dysplasia-fmd (Accessed: 25 January 2022).
"Fibromuscular Dysplasia: Practice Essentials, Background, Pathophysiology" (2021). Available at: https://emedicine.medscape.com/article/1161248-overview#showall (Accessed: 25 January 2022).


This podcast sponsored by:
About Anatomy Trains:
Anatomy Trains is a global leader in online anatomy education and also provides in-classroom certification programs forstructuralintegration in the US, Canada, Australia, Europe, Japan, and China, as well as fresh-tissue cadaverdissectionlabs and weekend courses. The work of Anatomy Trains originated with founder Tom Myers, who mapped the human body into 13 myofascial meridians in his original book, currently in itsfourthedition and translated into 12 languages. The principles of Anatomy Trains are used by osteopaths,physicaltherapists,bodyworkers,massagetherapists,personaltrainers,yoga,Pilates,Gyrotonics,and other body-minded manual therapists and movement professionals. Anatomy Trains inspires these practitioners to work with holistic anatomy in treating system-wide patterns to provide improved client outcomes in terms of structure and function.
Website:anatomytrains.com
Email:info@anatomytrains.com
Facebook:facebook.com/AnatomyTrains
Instagram: instagram.com/anatomytrainsofficial
0:00:01.2 Ruth Werner: Hey, "I Have a Client Who... " listeners, did you know I have a growing library of NCB approved one-hour online self-paced continuing education courses that you can do any time, anywhere. Well, now you know. Current classes include What's Next, COVID-19 updates for Massage Therapists and A Massage Therapist's Introduction to Pharmacology Part One, and brand new, A Massage Therapist's Introduction to Pharmacology Part Two. Classes are $20 each and they confer one hour of continuing education credit. Wanna know more? Visit my website at ruthwerner.com and check it out. Be sure to sign up for my mailing list so you'll never miss a new class.
0:00:47.5 Speaker 2: Anatomy Trains is thrilled to announce our first ever women's health symposium. This live online event takes place February 26 and 27, 2022 AWST, that's Australian Western Standard Time. Register by January 21st to receive a significant early bird discount and over $400 worth of bonuses. We have invited a powerful line-up of all female authors, physicians, therapists and clinicians to share their passion and life's work. Visit anatomytrains.com for details.
[music]
0:01:35.9 RW: Hi, and welcome to "I Have a Client Who... " Pathology Conversations with Ruth Werner, the podcast where I will discuss your real life stories about clients with conditions that are perplexing or confusing. I'm Ruth Werner, author of A Massage Therapist's Guide to Pathology. And I have spent decades studying, writing about and teaching about where massage therapy intersects with diseases and conditions that might limit our client's health. We almost always have something good to offer even with our most challenged clients, but we need to figure out a way to do that safely, effectively and within our scope of practice, and sometimes as we have all learned, that is harder than it looks. Today's episode comes from a massage therapist in Calgary who sent me a great topic, but rather than jumping right to her story, let's try this, which is not the description our contributors sent, but it's a good starting place that will start some wheels rolling. So here it is, let's say you have been seeing a client occasionally for several years, she is a 42-year-old mother of three, she has no history of significant health issues. Today, she comes in and she has been having some dizziness or maybe it's vertigo. She doesn't really know the difference. And it's been going on for a few days. Her low grade tinnitus has turned up loud, she can hear her own pulse in her ears, her headaches have gotten more severe and more frequent.
0:03:13.1 RW: This morning, she had this crazy new neck pain along with her headache, it's like nothing she's ever had before. Oh, and by the way, her low back pain is really flared up too. She is so glad she has this session scheduled, she cannot wait to get on your table. Okay, let's think about that for a minute. Dizziness or vertigo, worsening headache, tinnitus, I don't know. Could be sinus congestion or stress. Nothing sounds really scary here, but I hope your eyes pricked up at the neck pain thing. Still non-specific, but it's out of this general stress-related symptom pattern. And what about that low back pain, is that part of this or is that just incidental? Well, here's the kicker. If this woman went to her doctor, she would probably find out that her blood pressure is suddenly much higher than usual, high enough to damage her blood vessels and that pain in her neck, that's a situation called SCAD sudden carotid artery dissection and that is not great news. What if you had done some deep work along her sternocleidomastoid muscles to try to get ahead of those headaches or the low back pain, maybe is muscular. Or it could be that her renal arteries are so narrow that her kidneys are sending pain messages.
0:04:42.7 RW: Yikes, right? But there's more. So now I will share the story, our contributor sent. She says, "I just had another interesting condition I've never heard of, and it's not even in your book, are you interested? Fibromuscular dysplasia. The client is open to sharing it as it can display some very common symptoms that we see in the massage room, also any guidance with continued safe massage for her would be appreciated. She's cleared for light exercise, her physiotherapist suggested some massage, she had to have two surgeries on her kidney due to complications three months ago, she has high blood pressure as a result of all of this. It is being controlled. I did give her a very gentle relaxation massage, but any advice would be greatly appreciated if she books back in. Aha! Fibromuscular dysplasia. I don't often get the chance to dive in on a topic about which I know nothing, so this is gonna be fun. Before we proceed, let's take this name apart a little bit, it doesn't look hard, fibromuscular. Okay, muscle fibers, check. Dysplasia, that sounds like bad formation. Actually, I cheated and looked up this etymology just to be sure I got it exactly right.
0:06:07.6 RW: So without any more information, my prediction is that fibromuscular dysplasia or FMD is a disease involving some problems in the formation of muscle fibers. And because I've never heard of it and muscle fibers are in our bailiwick, I will guess that FMD must be really rare. Well, I got that last part, right? According to the website at Johns Hopkins, and if you do the kind of work I do, you will know that practically the same paragraphs show up in multiple locations. Fibromuscular dysplasia is "A rare blood vessel disorder in which some of the strong flexible cells of arteries are replaced with cells that are more fibrous, fibrous cells are less strong and also less flexible. This change in the composition of the arteries leads to their becoming stiffer and more prone to damage. FMD can lead to high blood pressure, stenosis, aneurysm, and sometimes dissection of the arteries." Oh, well, that sounds intense. And also it sounds nothing like what I thought. The muscle fibers it refers to are smooth muscle cells of the artery, so this is a vascular disease not a skeletal muscle problem. But while it is often sub-clinical, that means it creates no symptoms and doesn't require treatment, sometimes FMD can be very serious indeed.
0:07:38.9 RW: Okay, so some smooth muscle cells are replaced with fibrous cells that are not as strong or as elastic, and the result of this is two bad things. This section of artery can close in and get really tight, that's stenosis, but it is also structurally weak, which means it's at risk for bulging into an aneurysm and the whole system gets much tighter leading to high blood pressure, which is an extra dangerous situation for someone who has aneurysms that might rupture. What causes those muscle cells to change with FMD? Truthfully, no one knows. It sometimes appears to have a genetic component, as some families seem especially prone to this kind of weird arterial problem. It's diagnosed most often in women of childbearing age, so one theory is that it has something to do with hormone secretion. However, it is not statistically linked to any specific child-bearing history, and it is occasionally seen in males and young children, so the role of hormone cycles is probably not essential. We've identified three subtypes of FMD, intimal fibroplasia, medial fibroplasia and adventitial fibroplasia. I hope these terms sound familiar. Of course, the intima is the inside of our blood vessels, and FMD that affects this layer is very rare.
0:09:13.0 RW: The adventitia is the outer layer of our blood vessels. Adventitial fibroplasia is also very rare. The vast majority of cases affect the tunica media, that's medial fibroplasia, and it's the middle muscular layer of blood vessels, and even then, it's not what you would call a common condition. Random autopsy reports suggest that FMD might occur in something like 0.02% of the population, but really, no one is very sure about this number. The arteries most at risk for FMD are the renal arteries and the arteries that supply the brain, including the carotid and vertebral, and sometimes the cerebral arteries that are up inside the brain. Some patients have damaged areas in their mesenteric arteries that go to the intestines or to the major arteries that go to the extremities, and most patients have FMD in more than one location. So here we are with this weird idiopathic disorder that involves structural weak points in what are called the medium-sized arteries, and this disorder can cause hypertension and vascular damage like aneurysms and worse, but this is often silent, so how does a person know if they have it? Well, often FMD is found by accident when a person is being tested for something else, but sometimes they find out when blood vessel damage has progressed to the point of being dangerous.
0:10:43.9 RW: Signs and symptoms of FMD in the head and neck include increased headaches and migraines, and a situation called pulsatile tinnitus, where we can hear our pulse as a beating in our ears. If a carotid artery has dissected, then a sudden onset of neck pain that might ring a bell because I've just described our first scenario, our fictional 42-year-old mother of three. Let's just take a second to define what a dissected artery is, 'cause it might sound like the artery is actually split open and blood is pouring out of it, and that's not quite right that would be a ruptured artery. A dissected artery is a kind of aneurysm, a big bulging, weak spot. In this case, there's been a split, a dissection between two or more walls inside the artery, in other words, the tunica intima has split from the tunica media and blood pools in that in-between space. This artery is now much narrower than it was before, and it is much weaker, and the blood that lingers and that split off area will congeal into a big old clot or collection of clots, so the artery is occluded and if any clot fragments travel, they will cause an infarction. And if this is happening in the carotid artery, we are talking about a stroke.
0:12:06.8 RW: This actually gives us a bit of a hint about FMD. If a person under 50 who has no particular risk factors has a stroke or even a TIA, a transient ischemic attack, or a mini-stroke. Or if they have a condition called Bruit, that's B-R-U-I-T, which is a special sound that can be heard with a stethoscope and it's made by occluded blood vessels, well, that is a reason to investigate the possibility of fibromuscular dysplasia. If the renal arteries are the main target, then the main thing that will happen is that blood pressure will rise and the kidneys will function less efficiently. Interestingly, FMD does not usually lead to renal failure, but let's do be aware that kidneys can refer pain to the low back, and that is something for us to keep in mind. The kicker here is that all of these tissue changes develop, but it is completely independent of cardiovascular disease, that is to say atherosclerosis and the occlusion of blood vessels with atherosclerotic plaques is not a factor in FMD.
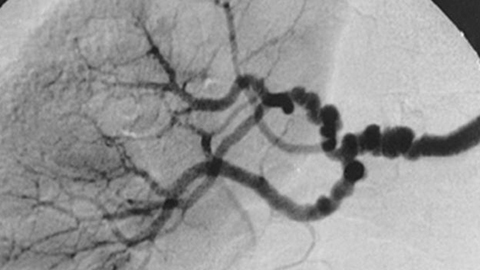
0:13:18.8 RW: So this condition is usually diagnosed with the use of imaging, including computed tomography and geography, that's a CTA or specialized ultrasound or some other kinds of tests. FMD has a particular appearance in the arteries that it effects, it makes these tight spots and these little aneurysms so what you get are several bulges in a row that looks like a string of beads. The Cleveland Clinic article that I used to help me get this information has a gorgeous example of this image, and you'll find a link to it in the show notes, I promise, it is worth a look. It's worth pursuing a diagnosis if someone is having these signs and symptoms, because FMD can look like some other things. It can look like typical atherosclerosis with hypertension, it can look like a sub-type of Ehlers-Danlos syndrome that also involves weakened blood vessels or another inherited connective tissue disorder called Marfan syndrome.
0:14:17.7 RW: And all of these have different treatment options and very different implications for the patient. If FMD causes symptoms, then it probably requires intervention. For our focus is first and foremost on managing hypertension to prevent any further damage to blood vessels, and this can be done with a combination of anti-hypertensive drugs, quitting smoking if that's an issue and instituting a low salt diet and appropriate exercise. Patients might be prescribed anti-platelet medication, especially if any stenosis is found in the arteries of the neck and head, and if arteries are dangerously narrowed, then some kind of surgical intervention might be required. Often this means some version of balloon angioplasty for the renal or carotid arteries, possibly a stent might be inserted to keep the artery widened and in very extreme cases, the whole artery might be reconstructed or bypassed.
0:15:16.4 RW: People with FMD are also encouraged to get imaging tests yearly or more often if they develop new symptoms. Okay, that was a lot of information about a very rare condition that most massage therapists will probably never deal with, but it's relevant because as our contributor noticed the signs and symptoms are the sort of things we might see a lot, headache, back pain, neck pain. So let's return to our client to review, she was diagnosed with FMD, she's cleared for light exercise, her physiotherapist suggested some massage. That's a good sign. She's had two surgeries on her kidney due to complications and those surgeries happened three months ago, she has high blood pressure as a result of her condition, but it is under control. I'm gonna guess that the kidney surgeries had to do with her renal arteries, if it was a balloon angioplasty, that can be done without open surgery, so the risk of scarring and infection and other kinds of secondary tissue damage is much lower than if she needed something major like an arterial reconstruction.
0:16:27.5 RW: So let's think of some questions for this client, here are a few beyond the constant starting place, what would you like to accomplish with massage today? My questions might include, did you have open surgery for your kidneys? And what are the repercussions of that? Do you have fibromuscular dysplasia in any other arteries, especially around your neck? What are your goals with physiotherapy? Do you have any side effects from your medications, and tell me about your daily exercise and other activities. Let's remember that being cleared for exercise doesn't mean she actually is exercising, although it does mean she probably has some decent capacity for adaptation. Her blood pressure medications might make her feel a little logy, that's something we wanna anticipate, and if her anti-platelet meds are causing her to bruise easily, we wanna know that too.
0:17:22.3 RW: But there's one big thing we wanna know about massage for this person, remember, FMD almost always happens in more than one place and the carotid artery is at particular risk. This is a client who is not a good candidate for deep specific massage to the neck, especially around the sternocleidomastoid, which is the pathway of the carotid artery. Of course, if imaging tests have established that her carotid arteries are fine and healthy, that caution can be withdrawn, but we should probably revisit that from time to time. My words of advice, based on the way more than I thought it would be kind of information that I have pulled together on FMD include this, this client could be really eager for a lovely non-challenging, relaxing massage, and there's no reason she can't receive that with accommodations for her meds and the caveat that work on her neck needs to be extra cautious.
0:18:24.1 RW: I wanna give special thanks to this contributor who has actually provided fodder for a couple of other episodes of "I Have a Client Who... " And I wanna encourage you to do the same. Hey everybody, thanks for listening to "I Have a Client Who... " Pathology Conversations with Ruth Werner. Remember, you can send me your "I Have a Client Who... " stories to, ihaveaclientwho@abmp.com, that's ihaveaclientwho, all one word, all lowercase @abmp.com. I can't wait to see what you send me and I'll see you next time.
[music]